Glaucoma
Glaucoma is an eye disease in which the nerve fibers of the optic nerve gradually deteriorate. These optic nerve fibers normally direct the image that is formed by the eye to the brain, which tells us what the eye sees. The loss of optic nerve fibers creates blind spots (visual field defects) in the image. The ophthalmologist can detect the loss of optic nerve fibers because the optic nerve’s slowly starts to look different (the optic nerve is eroded: “excavated”).
If the disease is not or inadequately treated, the visual field will be damaged further and eventually the sharpness of your vision can also be affected.
Eye pressure
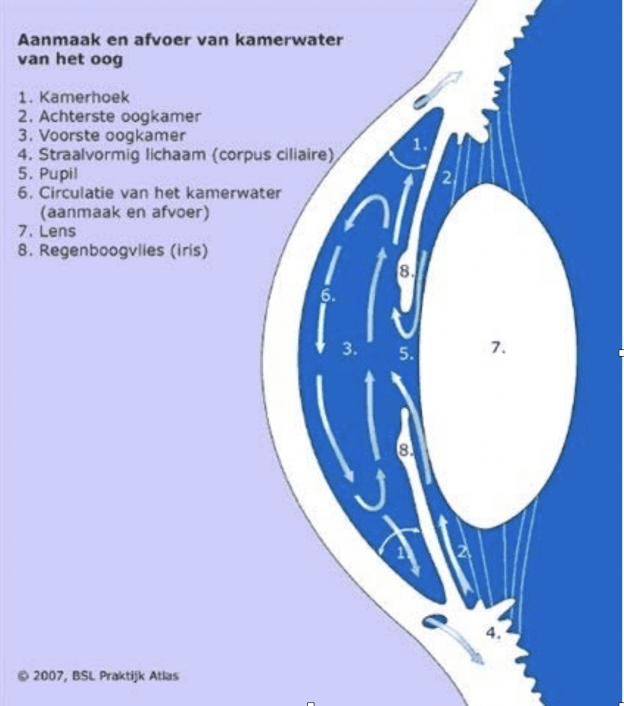
The spherical shape of the eye is also maintained because a moisture called aqueous humor is produced inside the eye. This eye fluid has nothing to do with tears, which are external. The level of eye pressure is set by the balance between production and discharge of the aqueous humor (see Figure 1). A raised eye pressure may occur when the discharge of aqueous humor is obstructed or the supply is too high. When the pressure becomes too high the optic nerve can be damaged.
Cause of glaucoma
We have not yet figured out in detail how this mechanism leads to damage of the optic nerve in glaucoma. However, there are many factors known to increase the risk of glaucoma significantly (risk factors):
- Raised eye pressure
This is by far the most important risk factor. Statistically, a normal eye pressure lies between 11 and 21 mmHg. The higher the eye pressure, the greater the risk of glaucoma. Yet, the majority of people with an eye pressure above 21 mmHg will not get glaucoma. - Heraditary glaucoma
If Glaucoma occurs in close (first and second degree) family members, chances of glaucoma are almost 10 times higher than for a person without Glaucoma running in the family. - Old age
In old age, glaucoma is much more common (4% of people over 80 suffer from glaucoma). - Severe near- or farsightedness
- Patients of African or Asian origin have an increased risk of glaucoma
- Abnormalities in the blood vessels at or in the eye
Types of glaucoma
Glaucoma is a common condition: 1.5% of Dutch people aged 40 and over have glaucoma. Glaucoma is classified into primary and secondary glaucoma. Primary glaucoma is a stand-alone disease without known cause. Secondary glaucoma occurs as a symptom in another (eye) disease, or through the use of certain medicines or eye drops.
Primary glaucoma is subdivided into:
1. open-angle glaucoma,
2. closed-angle glaucoma and
3. intermittent closed-angle glaucoma.
- Of the primary glaucomas, open-angle glaucoma is the most common, comprising high-pressure and normal-pressure glaucoma. In high-pressure glaucoma the drainage system of the eye gets clogged. This increases eye pressure and eventually damages the optic nerve, causing visual field defects. In normal-pressure glaucoma there are other risk factors, such as vascular blood circulation, that probably play a bigger role than the eye pressure, which is not raised. This form, too, causes optic nerve damage and loss of vision.
- In closed-angle glaucoma, the construction of the eye is such that access to the drainage system of the eye can get blocked by the iris, so the eye fluid cannot be discharged and the eye pressure is raised. This form of glaucoma can be acute or chronic. The acute form is rare and usually accompanied by blurred vision, a red eye, headaches, nausea and vomiting. These symptoms are caused by the extremely high eye pressure and quick treatment is necessary to prevent damage to the optic nerve. The chronic form is more common and can be treated well at an early stage. People who are farsighted, wearing strong plus prescription glasses, have more chance of getting this form of glaucoma. The eye lens will close the drainage angle. As the lens slowly thickens during one’s life, this condition mainly occurs from the age of 50.
- In intermittent closed-angle glaucoma, the corner of the room is closed sometimes. This can cause symptoms like headaches and will occur especially in the evening and at night. This can be considered a preliminary stage of closed-angle glaucoma. This condition hardly ever gets mentioned. However, we find that many patients with headaches and a narrow drainage angle recover from their headaches after an iridotomy.
Diagnosis
Ideally, everyone over 40 years old would get screened for glaucoma. However, not all glaucoma patients will be detected when eye pressure is the only aspect that is measured during examination. As becomes clear from the list of risk factors, glaucoma holds many more factors than eye pressure alone.
Therefore, apart from measuring the eye pressure, the optic nerve should be examined, a visual field test should be performed if necessary and/or the optic nerve should be X-rayed. If there is a suspicion of glaucoma after this examination, ophthalmologist and patient can decide together if and which form of treatment is needed. A glaucoma patient should be monitored for life.
Glaucoma treatment
Right now, the only proven therapy for glaucoma is lowering of the eye pressure. If the eye pressure is lowered sufficiently, a further increase in visual field defects is usually prevented. However, existing visual field defects can not be undone. That is why glaucoma must be detected at the earliest possible stage. Yet, not everyone with raised eye pressure is treated. There are people with (moderately) raised eye pressure that will not damage the optic nerve. These people do not have glaucoma but ocular hypertension. Treatment is unnecessary, but monitoring is required. Depending on possibly pre-existing risk factors for glaucoma, the ophthalmologist will discuss with the patient how often the eye pressure should be checked.
However, there are people with a regular eye pressure (<22 mmHg) who still have a damaged optic nerve. These people actually do have glaucoma and should be treated (normal-pressure glaucoma).
When treating people, eye drops are usually the first choice of treatment. There are many different types of eye pressure-reducing eye drops. The ophthalmologist will choose the type of eye drops that have a maximum eye pressure reducing effect combined with minimal side effects. The patient must turn the application of eye drops (once or several times a day) into a habit, so no eyedrops are forgotten. The technique for eye dropping can cause problems in the beginning. The patient must keep dripping until he feels a drop inside the eye. If eye drops remain hard to apply, an aid for this is available at the pharmacy.
In potential closed-angle glaucoma, laser is used to puncture the iris. This is a one-off treatment. In extreme cases, cataract surgery may be necessary.
In certain patients, laser treatment (SLT = selective laser trabeculoplasty) can be performed when the use of eye drops does not lower the eye pressure sufficiently. The laser light widens the drainage system of the eye fluid.
A final option is an eye pressure-lowering operation. This is referred to as a filtering operation during which either an extra drain is either created or implanted. Both surgery techniques have varying success. Unfortunately, there is no treatment with guaranteed success.
A recent development are tiny glaucoma implants (XEN implant) with the advantage that the burden on the eye is not so heavy. The disadvantage is that the effects are also quite subtle. These implants are not yet widely used.
The treatment of glaucoma remains highly customized.
Any questions? Please contact OMC Amstelland.
Source: NOG patientenvoorlichting | www.oogheelkunde.org
